Welcome to the Afibber’s Forum
Serving Afibbers worldwide since 1999
Moderated by Shannon and Carey
 |
 |
 |
 |
 |
 |
Home
>
AFIBBERS FORUM
>
Topic
Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score?
Posted by susan.d
|
Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 21, 2022 12:13AM |
Registered: 10 years ago Posts: 2,514 |
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 22, 2022 12:25AM |
Registered: 8 years ago Posts: 68 |
Related to this question:
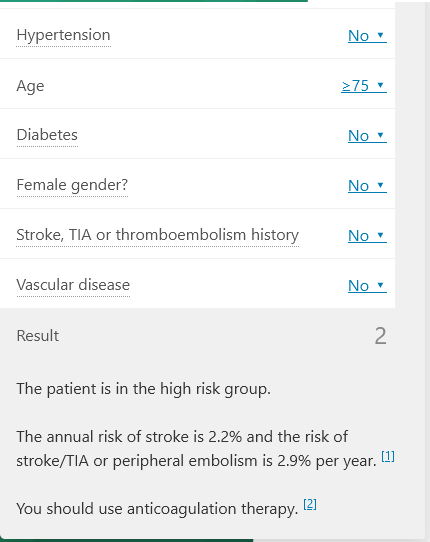
Does everyone in the world over 75 years old (male or female) with no other heart issues and no afib or diabetes be recommended to take an anticoagulant? The chart below would imply "yes".
Or, if you did have afib, but have had one or more ablations and are in NSR for a year or more, do you still have a vascular disease? And if not, would an anticoagulant still be recommended?
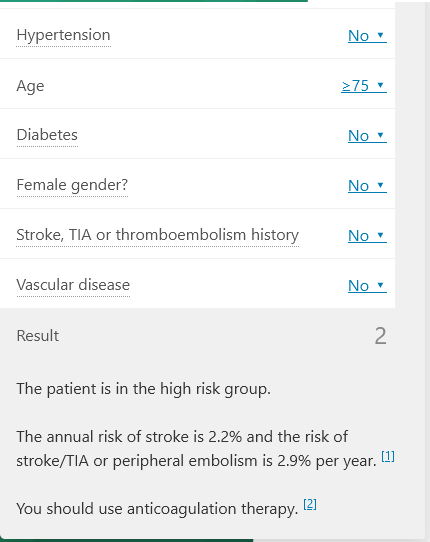
Does everyone in the world over 75 years old (male or female) with no other heart issues and no afib or diabetes be recommended to take an anticoagulant? The chart below would imply "yes".
Or, if you did have afib, but have had one or more ablations and are in NSR for a year or more, do you still have a vascular disease? And if not, would an anticoagulant still be recommended?
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 23, 2022 06:33AM |
Registered: 6 years ago Posts: 920 |
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 24, 2022 10:43AM |
Admin Registered: 6 years ago Posts: 5,336 |
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 24, 2022 11:19AM |
Registered: 8 years ago Posts: 68 |
We know the CHA2DS2-VASc score is used for people who have Afib. So anyone over 75 years old with Afib should be taking an anticoagulant.
So what is the definition of someone who has Afib? If they have an irregular heart beat then they are in Afib. But what if they have had one or more ablations and are in NSR for a year or more (5?) do you still have Afib and have to worry about a stroke?
While there is no cure for Afib, should you get credit in the CHA2DS2-VASc score for being completely in NSR for a period of time - like 5 years? And should the CHA2DS2-VASc score include a negative value for being in NSR, like -1?
And related to not being in Afib, what about after you have had a Watchman or similar device implanted in the LAA? Should you also get credit for that in the CHA2DS2-VASc score, like a -2?
Then we could rename the CHA2DS2-VASc score to CHA2DS2-VASc-NSR-LAAP (in NSR and have the LAA Plug) until we run out of letters?
So what is the definition of someone who has Afib? If they have an irregular heart beat then they are in Afib. But what if they have had one or more ablations and are in NSR for a year or more (5?) do you still have Afib and have to worry about a stroke?
While there is no cure for Afib, should you get credit in the CHA2DS2-VASc score for being completely in NSR for a period of time - like 5 years? And should the CHA2DS2-VASc score include a negative value for being in NSR, like -1?
And related to not being in Afib, what about after you have had a Watchman or similar device implanted in the LAA? Should you also get credit for that in the CHA2DS2-VASc score, like a -2?
Then we could rename the CHA2DS2-VASc score to CHA2DS2-VASc-NSR-LAAP (in NSR and have the LAA Plug) until we run out of letters?

|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 24, 2022 03:12PM |
Registered: 10 years ago Posts: 2,514 |
I believe Carey once wrote that one may have a successful ablation and in remission because there is no afib cure. With age and genetic disposition, one may get new firing pathways in areas of the heart that were not included in the pathways successfully fixed during the ablations. I could be wrong…
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 25, 2022 07:15AM |
Registered: 6 years ago Posts: 920 |
That's my understanding too.Quote
susan.d
I believe Carey once wrote that one may have a successful ablation and in remission because there is no afib cure. With age and genetic disposition, one may get new firing pathways in areas of the heart that were not included in the pathways successfully fixed during the ablations. I could be wrong…
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 25, 2022 08:44PM |
Admin Registered: 6 years ago Posts: 5,336 |
Yes, I did say that. An ablation puts a fence around the areas in your atria that are producing arrhythmic signals. If done correctly and competently, nothing within those fenced areas will ever be able to cause afib again. It doesn't matter what triggers you indulge in, those areas are silenced forever. But it is possible for new sources to arise outside those fences because afib is a progressive disease. There is more than one member here who has experienced this. The longest time span I know of is 12 years between successful ablation and reappearance of afib. (A second touch-up procedure with the same EP dealt with it easily.)
It's also true that people who have ever been diagnosed with afib have a higher stroke risk than those who haven't regardless of how long they've been in NSR. That's one of the many reasons why EPs have stopped using the term "lone afib" and have begun using the term "atrial myopathy" instead. "Lone afib" used to appear in this forum's title, and you might not have noticed but it no longer does and hasn't for a year or two now. Fact is, if you've ever been diagnosed with afib, you do have a form of structural heart disease and a higher stroke risk than people who haven't.
So the conclusion is it's not a simple question. If your CHADS score is 2 or higher for men and 3 or higher for women, I would be very careful about stopping anticoagulants even if you've been in NSR for years following an ablation.
Interesting question about what if you have a Watchman or similar device. I don't think there's data on that specifically yet and there probably won't be for years, but an LAA occlusion device returns your stroke risk to about the same as people who've never been diagnosed with afib, and many people do stop anticoagulants completely after receiving a device. So make your judgement calls. My personal decision was that half-dose Eliquis is safer and more effective than low-dose aspirin, which almost any doctor would prescribe for me given my age (66) and cardiovascular status, so I continue to take it despite being in NSR for 4 years and having a Watchman for 3 years.
It's also true that people who have ever been diagnosed with afib have a higher stroke risk than those who haven't regardless of how long they've been in NSR. That's one of the many reasons why EPs have stopped using the term "lone afib" and have begun using the term "atrial myopathy" instead. "Lone afib" used to appear in this forum's title, and you might not have noticed but it no longer does and hasn't for a year or two now. Fact is, if you've ever been diagnosed with afib, you do have a form of structural heart disease and a higher stroke risk than people who haven't.
So the conclusion is it's not a simple question. If your CHADS score is 2 or higher for men and 3 or higher for women, I would be very careful about stopping anticoagulants even if you've been in NSR for years following an ablation.
Interesting question about what if you have a Watchman or similar device. I don't think there's data on that specifically yet and there probably won't be for years, but an LAA occlusion device returns your stroke risk to about the same as people who've never been diagnosed with afib, and many people do stop anticoagulants completely after receiving a device. So make your judgement calls. My personal decision was that half-dose Eliquis is safer and more effective than low-dose aspirin, which almost any doctor would prescribe for me given my age (66) and cardiovascular status, so I continue to take it despite being in NSR for 4 years and having a Watchman for 3 years.
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 25, 2022 09:55PM |
Registered: 10 years ago Posts: 2,514 |
I have no problem taking a half dose Eliquis a day (with no baby aspirin) for life. I have a 3.5 month watchman. It’s stroke insurance. I witnessed one of my father’s strokes and it wasn’t a pretty sight. After a dozen major and mini strokes he was a vegetable. He was once a professional athlete. So think hard about stopping your NOAC. You would regret your decision if you get a stroke.
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 26, 2022 12:20AM |
Registered: 8 years ago Posts: 68 |
Thanks to Carey and Susan for that explanation. I have had afib for many years, am over 75 years old, had 2 successful Natale ablations, and been in NSR for over 2 years. That means, according to CHA2DS2-VASc, that I will be on an anticoagulant for the rest of my life. Even though I am in NSR now, afib and a stroke could return at any time.
But if I were to get a Watchman, I could go on a half dose of Eliquis per day. It would lower my risk of a stroke but I could still have one. Not sure how the insurance company would compare a Watchman procedure to saving a half dose of Eliquis per day for the rest of my life; I bet Eliquis would win. So we will have to wait some time for a study to positively prove that you can go off the anticoagulant after a Watchman. Not sure how an EP can recommend stopping the anticoagulant after the Watchman since there is no definitive study yet (except perhaps by the company?).
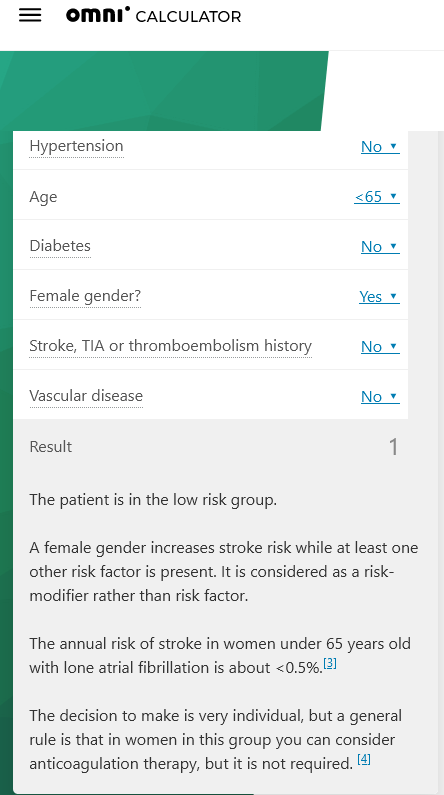
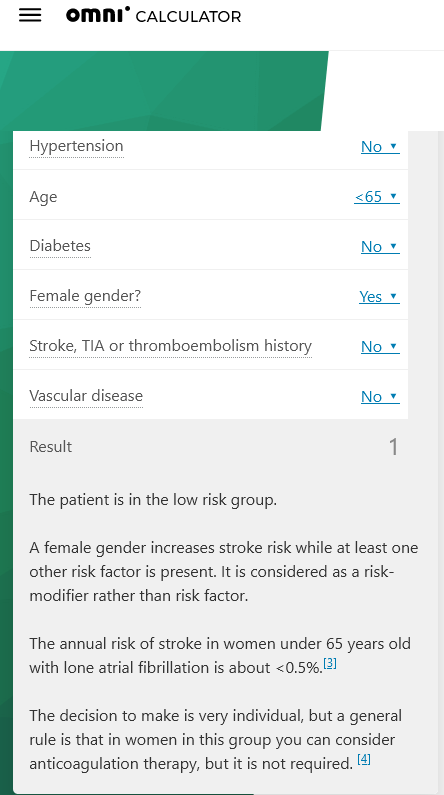
Back to Susan's question about the female sex attribute in the CHA2DS2-VASc score. I have read a lot of discussions and studies about removing the sex attribute from the score, but not seen a recent calculator that does this. I did find a few studies that thread the needle with the female sex. They say the female sex is a Risk Modifier rather than a Risk Factor in getting afib. The Omni Calulator (February 15, 2022, still threading the needle) keeps the female gender, but gives you the option of using it or not, depending if another Risk Factor is present. See below and their explanation:
But if I were to get a Watchman, I could go on a half dose of Eliquis per day. It would lower my risk of a stroke but I could still have one. Not sure how the insurance company would compare a Watchman procedure to saving a half dose of Eliquis per day for the rest of my life; I bet Eliquis would win. So we will have to wait some time for a study to positively prove that you can go off the anticoagulant after a Watchman. Not sure how an EP can recommend stopping the anticoagulant after the Watchman since there is no definitive study yet (except perhaps by the company?).
Back to Susan's question about the female sex attribute in the CHA2DS2-VASc score. I have read a lot of discussions and studies about removing the sex attribute from the score, but not seen a recent calculator that does this. I did find a few studies that thread the needle with the female sex. They say the female sex is a Risk Modifier rather than a Risk Factor in getting afib. The Omni Calulator (February 15, 2022, still threading the needle) keeps the female gender, but gives you the option of using it or not, depending if another Risk Factor is present. See below and their explanation:
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 26, 2022 03:08AM |
Registered: 6 years ago Posts: 920 |
I'd add that people at higher stroke risk are those having some undiagnosed form of SHD. When diagnosed, afib does not seem to increase stroke risk provided appropriate care is prescribed and followed.Quote
Carey
Fact is, if you've ever been diagnosed with afib, you do have a form of structural heart disease and a higher stroke risk than people who haven't.
I think afib is mostly associated with higher stroke risk because of people being diagnosed AFTER having had a stroke.
Both my parents were afibbers, but my father was diagnosed after a stroke. He had serious sequels and passed because of that. My mother left last year at 93, but her afib never caused her serious issues. She'd been diagnosed soon enough.
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 30, 2022 05:23PM |
Registered: 1 year ago Posts: 104 |
If you have had an LAA surgical closure how would that affect the score or risk? I had a mini maze procedure with a LAA closure - my surgeon explained to me that my risk for stroke was the same as any person not having afib - as long as I stayed in NSR. I asked the EP what he thought, and he was on the fence about it. I asked about a Watchman and he told me there was no room for it due to the closure. I know there is some research being done on this topic of surgical closure vs device. What is the point of LAA closure if you still need to take anti coagulant? There will never be 0 risk even if on the medications.
Dr. Wolf aka Wolf Mini Maze - in Texas has an opinion on this closure topic. According to the CHAD Vasc scoring system everyone over a certain age should be on an anti coagulant. There is no specific answer at this point. The Docs will mostly be on the conservative side. I am a health care worker, and I have treated stroke patients for years, many of them did not have AFIB. Some were on blood thinners. Other issues yes
I have not been on anti-coagulants for over 14 years. But given my current age, I am thinking about doing a 1/2 dose. My Cario would like me to take a low dose aspirin because of age related heart risk in general.
Dr. Wolf aka Wolf Mini Maze - in Texas has an opinion on this closure topic. According to the CHAD Vasc scoring system everyone over a certain age should be on an anti coagulant. There is no specific answer at this point. The Docs will mostly be on the conservative side. I am a health care worker, and I have treated stroke patients for years, many of them did not have AFIB. Some were on blood thinners. Other issues yes
I have not been on anti-coagulants for over 14 years. But given my current age, I am thinking about doing a 1/2 dose. My Cario would like me to take a low dose aspirin because of age related heart risk in general.
|
Re: Unequal prescription of anticoagulants among females and males with atrial fibrillation and similar stroke risk: Should we omit sex category from the CHA2DS2-VASc score? May 30, 2022 07:00PM |
Admin Registered: 6 years ago Posts: 5,336 |
Quote
sldabrowski
I had a mini maze procedure with a LAA closure - my surgeon explained to me that my risk for stroke was the same as any person not having afib - as long as I stayed in NSR.
That was the correct answer.
A half-dose of Eliquis or Xarelto could make sense. Not for atrial stroke prevention, but for prevention of stroke from all the other possible sources. You would be better off with a half-dose of Eliquis than low-dose aspirin because Eliquis is safer and more effective than aspirin. Its only downside is it's a lot more expensive.
Sorry, only registered users may post in this forum.